
Vancomycin, 500 mg orally or via nasogastric tube 4 times per day plus metronidazole, 500 mg intravenously every 8 hours (particularly if ileus is present)

If neither agent is available: metronidazole, 500 mg orally 3 times per day for 10 daysįidaxomicin, 200 mg orally 2 times per day for 10 days Vancomycin, 125 mg orally 4 times per day for 10 daysįidaxomicin (Dificid), 200 mg orally 2 times per day for 10 days Strength of recommendation/quality of evidence * The choice of diagnostic test depends on local preference, financial constraints, and volume of samples tested each day. The EIA for toxins A and B has the highest specificity, whereas NAAT is both sensitive and specific. The EIA for GDH has high sensitivity, which makes it a useful screening test because a negative result essentially rules out infection (negative predictive value = 94% to 100%). 21 Nucleic acid amplification testing (NAAT) detects genes that encode the toxins, but it cannot distinguish colonization from active infection. Other diagnostic tests include enzyme immunoassay (EIA) for toxins A and B and for glutamate dehydrogenase (GDH), an enzyme made by all C. The reference tests with which other assays are compared include cell cytotoxicity neutralization assay and toxigenic culture, both of which have relatively long turnaround times and are thus rarely used in clinical practice. difficile infection is low, no diagnostic test should be used alone because of low positive predictive values. Guideline recommendation based on low- to moderate-quality longitudinal cohort studies

6, 27, 28īased on practice guidelines and consistent findings from small randomized controlled trials evaluating diarrheaĪntibiotic stewardship reduces rates of C. difficile infection in whom appropriate antibiotic therapy has been ineffective. Recommendation from an evidence-based practice guideline and large disease-oriented studyįecal microbiota transplantation is recommended for patients with multiple recurrences of C. Oral vancomycin and fidaxomicin (Dificid) are preferred over metronidazole for initial episodes of C. Guideline recommendation based on low-quality, small diagnostic studies
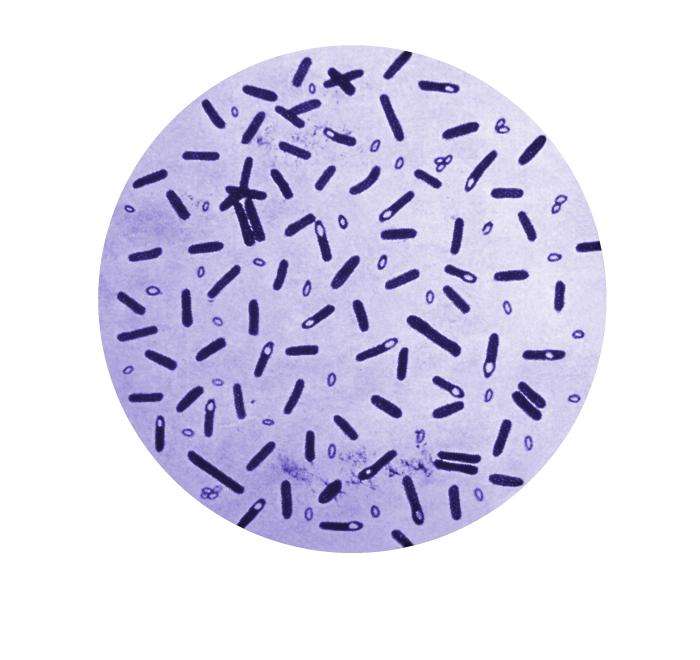
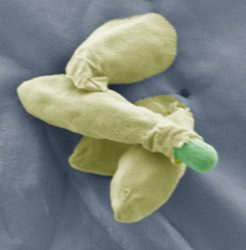
difficile infection based on clinical symptoms, either nucleic acid amplification testing or the two-step algorithm is appropriate. difficile infection.Ī two-step algorithm should be used to guide diagnostic testing for Clostridioides difficile infection: enzyme immunoassay for glutamate dehydrogenase and toxins A and B, followed by nucleic acid amplification testing if initial results are indeterminate. The Infectious Diseases Society of America does not recommend the use of probiotics for prevention of C. In routine or endemic settings, hands should be cleaned with either soap and water or an alcohol-based product, but during outbreaks soap and water is superior. Good antibiotic stewardship is a key strategy to decrease rates of C. Fecal microbiota transplantation is a reasonable treatment option with high cure rates in patients who have had multiple recurrent episodes and have received appropriate antibiotic therapy for at least three of the episodes. Metronidazole is no longer recommended as first-line therapy for adults. difficile infection, oral vancomycin or oral fidaxomicin is recommended. recurrent infection and on the severity of the infection based on white blood cell count, serum creatinine level, and other clinical signs and symptoms. Treatment depends on whether the episode is an initial vs. In children older than 12 months, testing is recommended only for those with prolonged diarrhea and risk factors. Testing in these patients should start with enzyme immunoassays for glutamate dehydrogenase and toxins A and B or nucleic acid amplification testing. difficile infection should be considered in patients who are not taking laxatives and have three or more episodes of unexplained, unformed stools in 24 hours. difficile infection is characterized by a wide range of symptoms, from mild or moderate diarrhea to severe disease with pseudomembranous colitis, colonic ileus, toxic megacolon, sepsis, or death. Risk factors include recent exposure to health care facilities or antibiotics, especially clindamycin. Guidelines for the diagnosis and treatment of Clostridioides difficile infection have recently been updated.


 0 kommentar(er)
0 kommentar(er)
